There are many reasons why your skin around the stoma can get red and sore. Some of them include irritation from stool, sensitivity/allergy to products you use like cleanser or moisturizer, yeast infection (Candidiasis). Below is a discussion of each one’s characteristics!
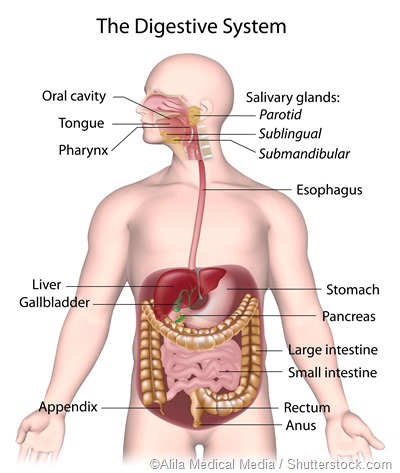
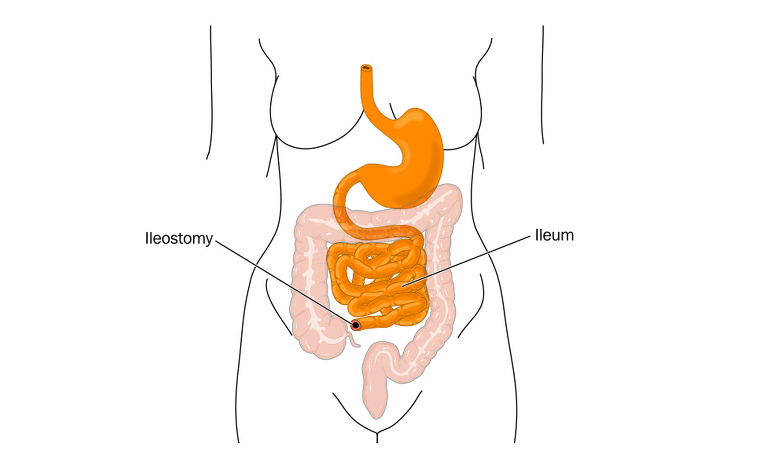
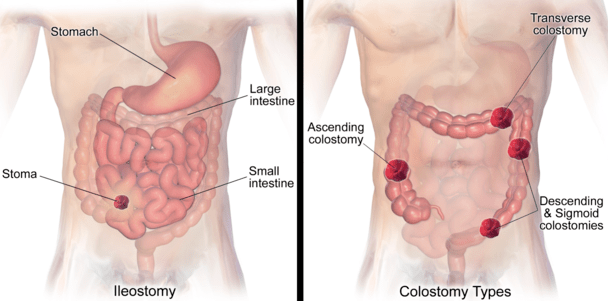
The most common cause of redness to the skin surrounding an ileostomy is stool coming into direct contact with it. The Corrosive effect from this type of digestive system can lead to pain and permanent damage if left untreated for too long or repeated exposure. You may notice small amounts of blood when the irritation has been present for a prolonged period because bacteria start eating away at damaged cells, which release chemicals similar enough that they’ll feel like pricking your finger on anything metal-like (i.e., sink drain).
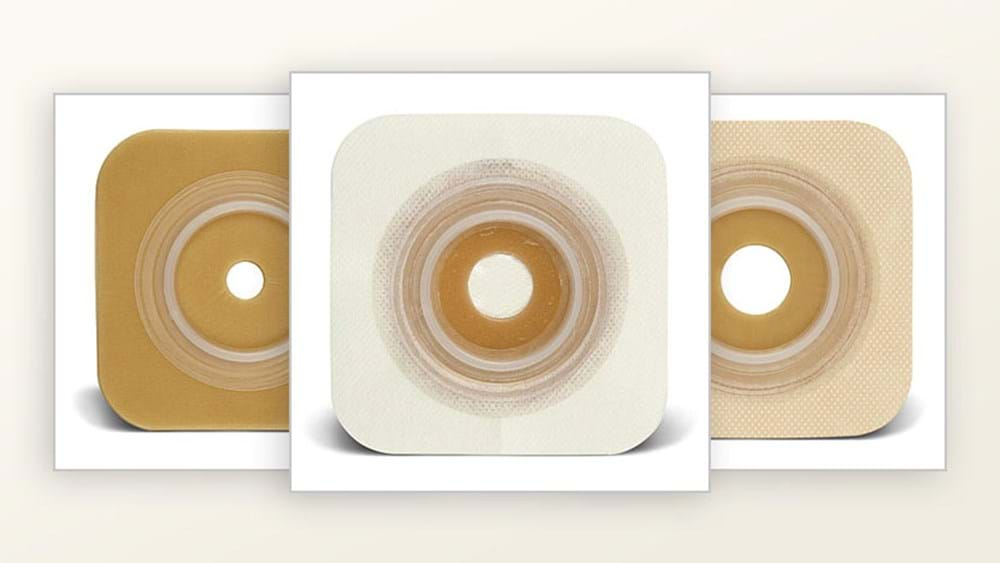
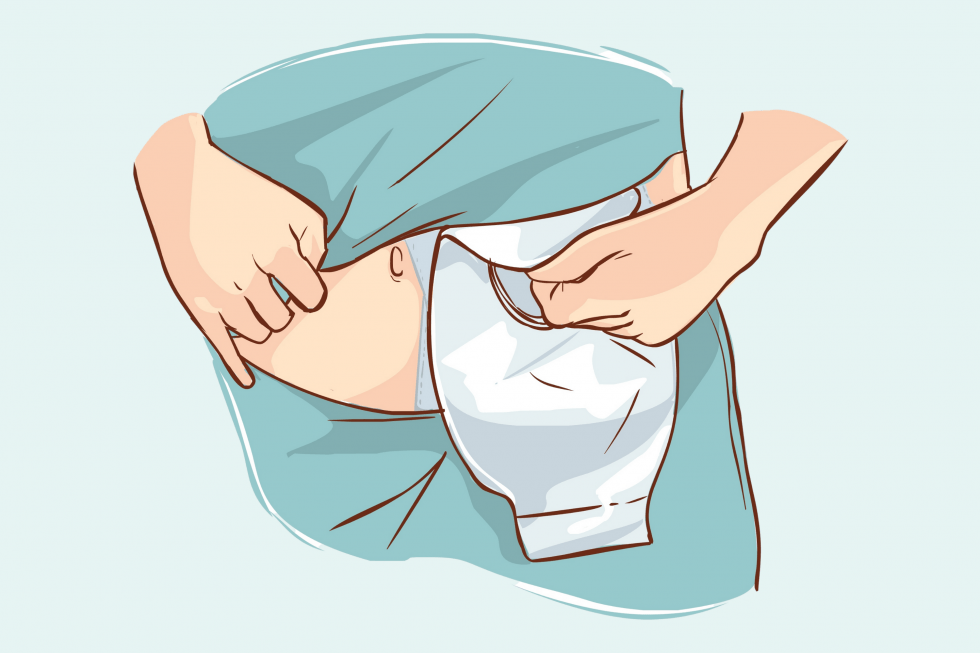
Ostomates often experience skin irritation from the stool, but it is possible to reduce this by using an appliance with a smaller opening. Suppose you have just one small hole in your ostomy for stoma accessories like buttons or strings of tapes. In that case, that will work fine and provide adequate protection against odors caused by bacteria on hands when handling waste products afterward.
The most common issue reported about Ostomy appliances is openings larger than expected which expose more peristomal skin preventing proper barrier function alongside paste use where too much material may enter through these holes, especially if there isn’t enough space between fingers.

Contact lenses can be uncomfortable and cause skin irritation. In the wrong size, shape, or position, they may also allow stool to leak under your appliance, causing contact with sensitive areas of your body, such as around the stoma site where there are folds in clothing that touch it. You could require a different type of retainer (e.g., maybe switching from flat flange rimmed with silicone gel rings onto a convex-shaped plastic frame). However, this will not always solve all problems associated with wearing them! It is essential when deciding on substitutes, remember they have limited capacity compared to soaps/washes; anything else put back into your diet must meet specific criteria.
The redness you are experiencing could be due to a range of factors, including an ingredient sensitivity or actual allergy. The borders on reactions often mimic what product has caused it; for example, if there is irritation near where tape touches the skin, this would only manifest under the barrier layer (tape). For more information about ostomy care, click here! The redness and itchiness of the skin may be due to a yeast infection. A rash will have bright red borders or edges, with irregularly-spaced pink dots all over them (satellite lesions). These are areas where new growth has appeared because of an increase in Yeast population near moist places like under ostomy appliances worn after taking antibiotics. Arglaes® is a silver-based powder that can be applied to the skin and stay on for two weeks. Suppose you don’t “seal” your Arglaes®. In that case, it will not stick properly, so make sure when using this product that there are no wrinkles or creases where the fungus may accumulate because they won’t get affected by any cream-based anti-fungal preparations either! Some people are more susceptible to yeast infections around the area where they have an ostomy. This is because clothes can’t fully cover it like other parts of their body, making these areas easier targets for fungus growths, and creams often don’t work as well here since there’s no skin barrier present. Meanwhile, if you notice redness elsewhere (such as under breasts), then consider switching products or using one with anti-fungal properties—though neither course will completely get rid of all signs unless treated professionally!

Redness around the stoma is typically caused by stool irritation, product sensitivity, and yeast. However, other reasons can account for redness. You should consult with an ET so they can adequately evaluate any symptoms you are experiencing!